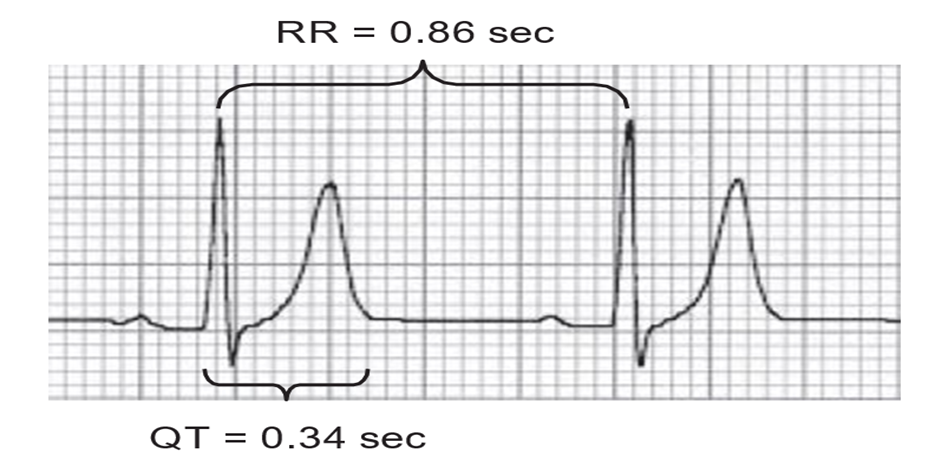
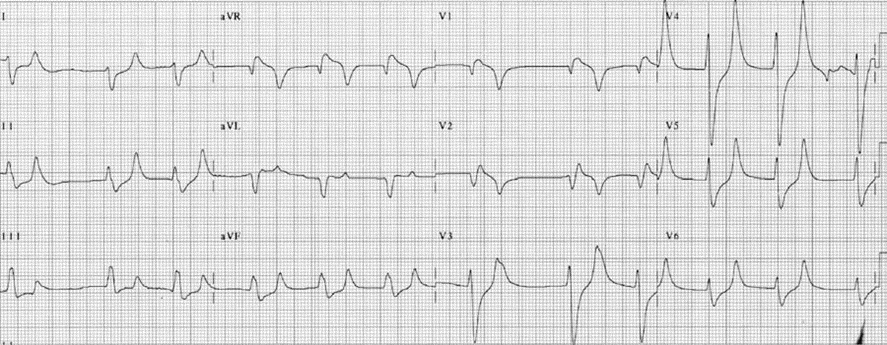
Among the various electrolyte abnormalities, hyperkalemia, hypokalemia, hypercalcemia, and hypocalcemia are the only disorders that can cause reliable diagnostic changes in the electrocardiogram (ECG). These ECG changes can be recognized well before the results of the laboratory tests become available. The severity of these electrolyte abnormalities usually parallels the changes in the ECG. A simple rule to remember regarding the effect of these electrolyte abnormalities on the ECG is that when increased levels are present (hyperkalemia or hypercalcemia), the QT interval is shortened. Inversely, when decreased levels of these electrolytes are present (hypokalemia or hypocalcemia), the QT interval is prolonged.
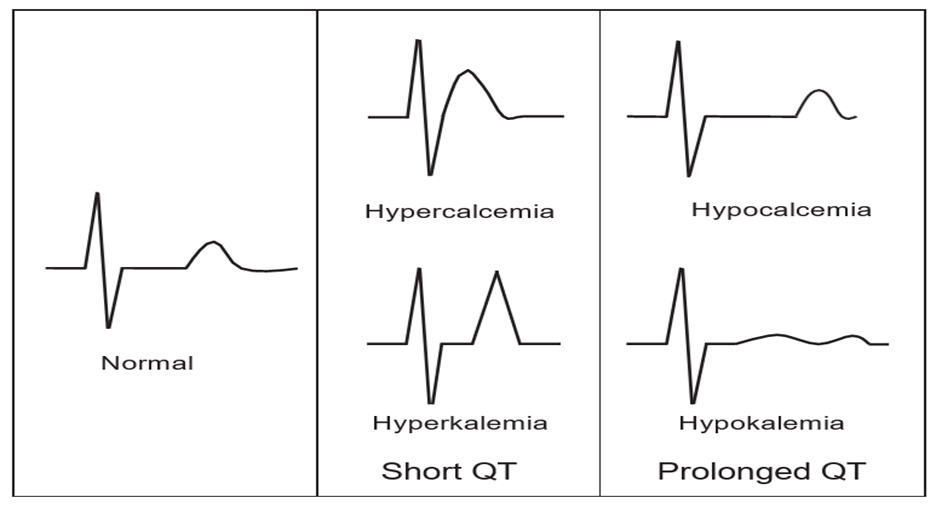
Figure 1 shows the ECG abnormalities associated with each of these electrolyte disorders.
The normal level of serum potassium varies from 3.3 to 5.3 millimoles per liter (mmol/L), also expressed as milliequivalents per liter (mEq/L). Hyperkalemia implies the presence of higher-than-normal levels of serum potassium.
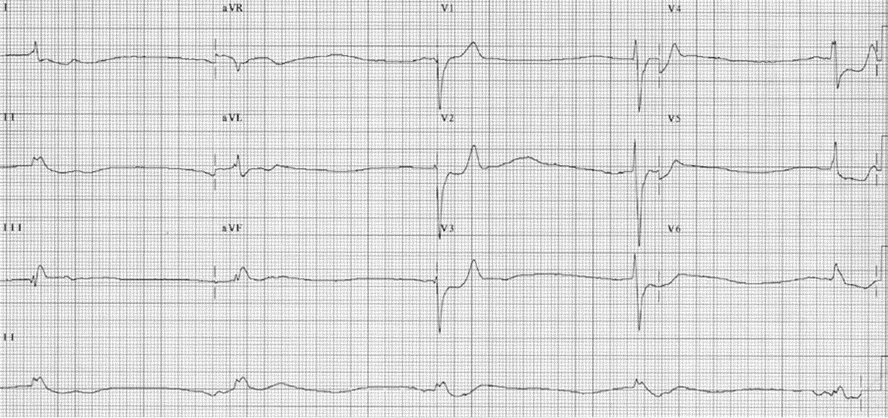
Among the electrolyte disorders, hyperkalemia is the most fatal. It also exhibits the most remarkable changes in the ECG. The ECG abnormalities generally reflect the increasing severity of the hyperkalemia, thus the ECG is useful not only in the diagnosis of this electrolyte disorder, but is also helpful in determining the intensity in which hyperkalemia should be treated.
Mild hyperkalemia (<6.0 mmol/L)
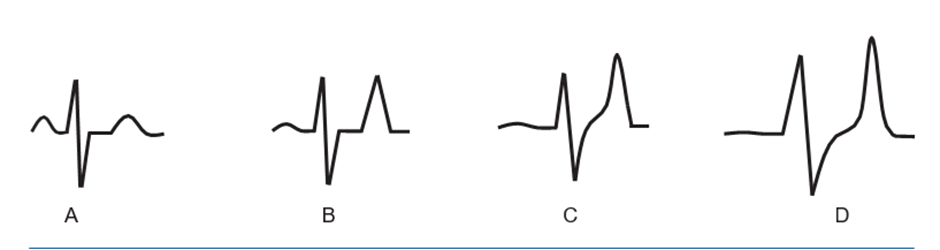
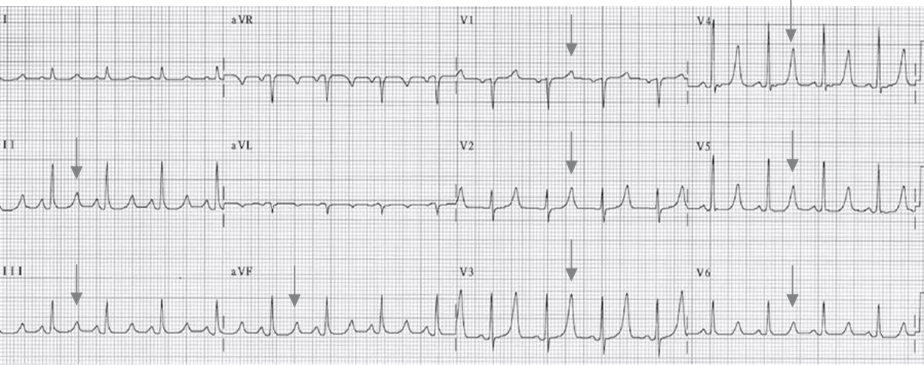
Peaking of the T waves occurs and may be the earliest and only abnormality that can be recognized. The QT interval is normal or shortened (Fig. 2B). Peaking of the T waves is the earliest to occur and is the most characteristic ECG pattern of hyperkalemia. Hyperkalemic T waves are often described as “tented” because they closely resemble the shape of a tent. The T waves are tall and symmetrical with a pointed tip and a narrow base (Fig. 25.3–25.5). The QT interval is generally short, unless coexisting abnormalities such as hypocalcemia or myocardial disease are present.
Moderate hyperkalemia (6.0 to 7.0 mmol/L)
More pronounced peaking of the T waves occurs, QRS complexes widen, P waves become broader with diminished amplitude, and PR interval lengthens resulting in atrioventricular (AV) block (Fig. 25.2C). As
the level of serum potassium increases, the amplitude of the T wave also increases and often the height of the
T wave becomes taller than the R wave. The T waves are tallest in precordial leads V2–4, because of the proximity of these leads to the myocardium (Figs. 25.5–25.7).
The onset of the P wave and QRS abnormalities is more difficult to predict than the T wave changes. In general, the P waves and QRS complexes start to widen when moderate hyperkalemia is present, as conduction through the atria and ventricles becomes delayed (Fig. 25.7).
Severe hyperkalemia (>7.0 mmol/L)
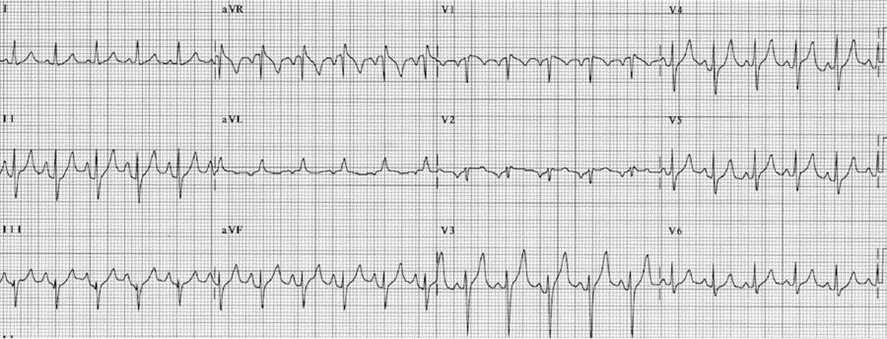
P waves become unrecognizable, further widening of the QRS complex occurs, S and T waves merge with a very short ST segment resulting in a sinusoidal wave, ST segment may be elevated in V1–2 and mistaken for acute ischemic injury, and, finally, slowing of the heart rate, asystole, or ventricular flutter can occur.
When the potassium level increases to “7.0 mmol/L, the amplitude of the P wave decreases until the P waves are no longer detectable. The absence of P waves in spite of normal sinus rhythm is due to marked slowing of the sinus impulse across the atria or the sinus impulse traveling through specialized internodal pathways.
Sinoventricular rhythm is the term used to describe sinus rhythm without any discernible P waves.
Sinoventricular rhythm is impossible to distinguish from junctional rhythm when the QRS complexes are
narrow or from accelerated ventricular rhythm when the QRS complexes are wide. Other ECG changes associated with severe hyperkalemia are shown in Figs. 7 through 15:


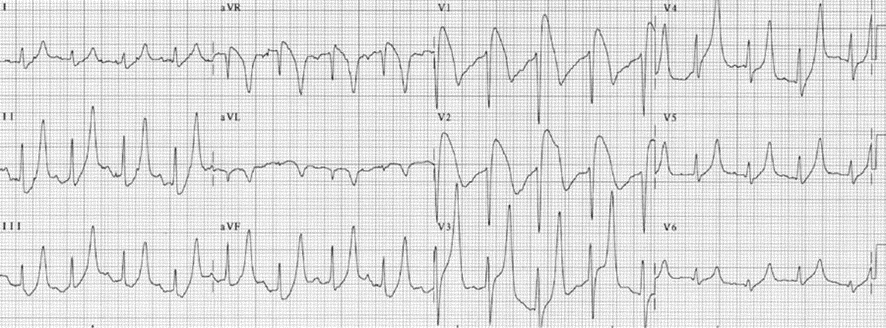

9.0 mmol/L. P waves are absent and the QRS complexes are wide with a left bundle branch block configuration. The rhythm is often called sinoventricular, although this is difficult to differentiate from accelerated idioventricular rhythm.
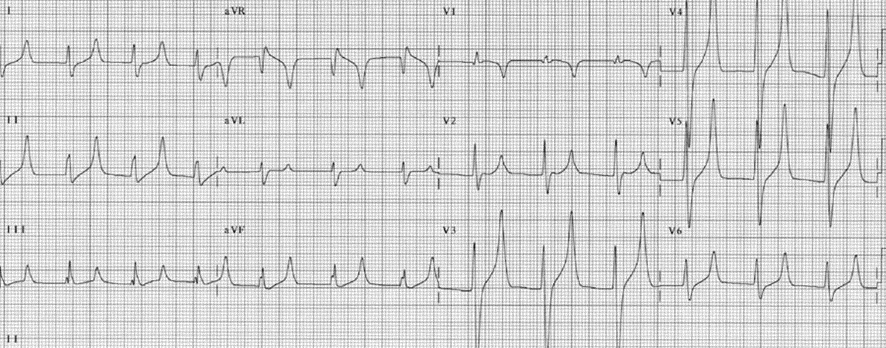
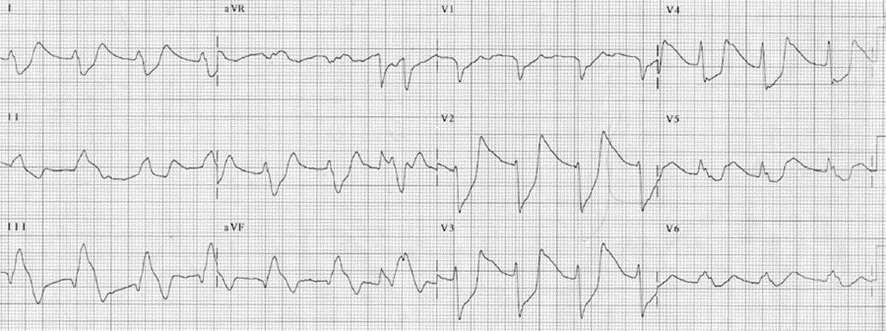
Potassium level is >10.0 mmol/L.
Other ECG changes associated with severe hyperkalemia are:
Further widening of the QRS complex, shortening of the ST segment and fusion of the S wave with the
T wave resembling a sine wave (Figs. 7, 12, and 13).
P waves completely disappear in spite of the rhythm being normal sinus, resulting in sinoventricular rhythm (Figs. 8, 10–15).
ST segment elevation mimicking acute ischemic injury can occur, especially in the right sided precordial leads V1–2 (Fig. 9).
Severe bradycardia (Figs. 10–15) or ventricular flutter/fibrillation may occur.

A Summary of ECG Findings of Hyperkalemia
- Increased amplitude and peaking of the T waves. This is the earliest, most consistent, and most characteristic ECG abnormality associated with hyperkalemia. T-wave peaking persists and worsens with increasing levels of hyperkalemia.
- The QT interval is short or normal.
- As hyperkalemia worsens, the QRS complexes widen.
- The P wave becomes broader and the amplitude becomes lower.
- AV conduction becomes prolonged.
- The P waves eventually disappear resulting in sinoventricular rhythm.
- The S wave continues into the T wave resulting in a sine wave configuration.
- Cardiac arrest from marked bradycardia, asystole, or ventricular flutter/fibrillation.
Clinical Implications of Hyperkalemia
- Potassium is the major intracellular ion in the body. Approximately 98% of the total amount of potassium is intracellular and the remaining 2% extracellular. This difference in concentration between intracellular and extracellular potassium is due to the presence of sodium potassium adenosine triphosphatase pump where 3 units of sodium is pumped out of the cell in exchange for 2 units of potassium. The ratio between intracellular and extracellular potassium makes the resting membrane potential negative at approximately –90 mV.
- Increased extracellular potassium may be due to increased potassium load, worsening renal function, or acute shift of intracellular potassium extracellularly. Increased potassium in the diet by itself rarely causes hyperkalemia. Some drugs can also cause hyperkalemia when there is renal dysfunction. These include potassium supplements, potassium sparing diuretics (triamterene and amiloride), aldosterone antagonists (spironolactone and eplerenone), angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and nonsteroidal anti-inflammatory agents including the selective cyclo-oxygenase 2 inhibitors. More commonly, hyperkalemia is due to renal failure. It may also be the result of acute shift of intracellular potassium to the extracellular space as when cells are damaged from hemolysis or rhabdomyolysis. Acidosis can also cause a shift of H+ ions into the cell in exchange for potassium that moves out of the cell. For every 0.1 unit decrease in blood pH, the level of potassium in the serum increases by approximately 0.5 mmol/L.
- Among the electrolyte abnormalities, hyperkalemia causes the most remarkable ECG abnormalities. The ECG changes frequently parallel the severity of the electrolyte disorder. The expected ECG findings, however, may not correlate well with the potassium level because the effect of hyperkalemia on the ECG depends on several factors and not just the serum potassium level. These include the baseline level of potassium, the rate of rise of potassium in the blood, coexisting electrolyte abnormalities, coexisting metabolic abnormalities, and the presence or absence of myocardial disease.
- Mild or moderate hyperkalemia is usually asymptomatic. When significant hyperkalemia occurs usually >7.0 mmol/L, symptoms include generalized weakness, paralysis, respiratory failure from respiratory muscle weakness, and cardiac arrest.
- Among all the electrolyte abnormalities, hyperkalemia is the most fatal. Because severe hyperkalemia can be diagnosed in the ECG, this will allow emergency treatment of the electrolyte abnormality even before the results of the laboratory become available.
- Similarly, the ECG is useful in the diagnosis of pseudohyperkalemia. The laboratory may mistakenly report a high potassium level not the result of actual hyperkalemia but from hemolysis after the blood is collected. If there are no associated ECG changes, the diagnosis of hyperkalemia is unlikely. This will obviate the need for unnecessary therapy.
Treatment of Hyperkalemia
Treatment should be tailored according to the severity of the hyperkalemia. The ECG abnormalities together with the serum potassium level serve as useful guide in dictating the intensity of management.
The American Heart Association (AHA) guidelines of cardiopulmonary resuscitation and emergency cardiovascular care recommend the following for the treatment of hyperkalemia.
1.Mild hyperkalemia, potassium level <6.0 mmol/L:
Potassium level <6.0 mmol/L is seldom of great concern. The only therapy that may be needed is to identify the cause of the hyperkalemia so that further increases in serum potassium can be prevented. In addition, therapy may include removal of potassium from the body.
- Loop diuretics: Furosemide 40 to 80 mg IV or bumetanide 1 mg IV to enhance excretion of potassium.
- Cation-exchange resin: Sodium polystyrene sulfonate (Kayexalate) is given orally or by retention enema. The oral dose can vary from 15 to 60 g daily. Fifteen grams is given orally one to four times per day. Sorbitol 20%, 10 to 20 mL is given every 2 hours or as needed to prevent constipation. Lower doses of Kayexalate of 5 to 10 g may be given up to three times per day without laxative therapy. If the patient is unable to take the resin orally, it can be given as retention enema, 30 to 50 g every 6 hours in a warm emulsion such as 50 mL 70% sorbitol mixed with 100 to 150 mL tap water and retained for at least 30 to 60 minutes. Each gram of Kayexalate removes approximately 1 mmol of potassium and takes at least 30 minutes to 2 hours to take effect. The resin binder carries a high sodium load and should be given cautiously to patients in congestive heart failure. The resin can also bind other cations such as magnesium and calcium. These electrolytes should be monitored together with the level of serum potassium. Patients on digitalis should be monitored closely since hypokalemia can aggravate digitalis toxicity.
2. Moderate hyperkalemia, potassium level 6.0 to 7.0 mmol/L:
When moderate hyperkalemia is present, therapy should be more emergent. In addition to eliminating the cause of the hyperkalemia and removal of excess potassium from the blood with loop diuretics and cation exchange resins, the level of serum potassium can be lowered more rapidly by shifting extracellular potassium intracellularly.
- Glucose plus insulin: Twenty-five grams of glucose (50 mL 50% dextrose) is mixed with 10 units of regular insulin. The solution is injected IV for over 15 to 30 minutes. Ten units of regular insulin can also be mixed with 500 mL 10% glucose. The solution is given IV for 60 minutes. The effect may last for 4 to 6 hours.
- Sodium bicarbonate: 50 mEq is given IV over 5 minutes. Sodium bicarbonate lowers extracellular potassium by shifting potassium into the cells. This agent is more effective when hyperkalemia is associated with metabolic acidosis. The effect may last for 2 hours and may be repeated as necessary.
- Nebulized albuterol: 10 to 20 mg nebulized over 15 minutes. B2 agonists shifts extracellular potassium intracellularly and the effect may last for ≥2 hours. If insulin is being given concomitantly, albuterol can attenuate its hypoglycemic effect.
3. Severe hyperkalemia and critical hyperkalemia, potassium level >7.0 mmol/L:
When serum potassium level exceeds 7.0 mmol/L or when the ECG abnormalities include absent P waves and changes in the QRS, ST segment and T waves, AV block or slowing of the heart rate, treatment of hyperkalemia should be very aggressive because severe hyperkalemia may cause lethal arrhythmias and cardiac arrest. The following agents are given in order of priority according to the AHA guidelines.
- Calcium chloride: 10% 5 to 10 mL (500 to 1,000 mg) given IV over 2 to 5 minutes. Calcium does not lower the level of serum potassium but will stabilize myocardial membrane against the toxic effects of potassium, thereby lowering the risk of fatal arrhythmias including ventricular fibrillation. The effect of calcium is immediate but lasts only for 20 to 40 minutes and repeated dosing may be needed.
- Sodium bicarbonate: 50 mEq given IV over 5 minutes. This should be injected using a separate tubing or IV line from that used for calcium chloride.
- Glucose plus insulin: Mix 10 units of regular insulin with 50 mL 50% dextrose. The solution is given IV over 15 to 30 minutes.
- Nebulized albuterol: 10 to 20 mg nebulized over 15 minutes.
- Loop diuretics: as above.
Kayexalate enema: 15 to 60 g plus sorbitol given orally or rectally as above.
Dialysis: If above therapy is unsuccessful, emergent dialysis should be considered especially in patients with renal failure even if not previously on dialysis.
Prognosis of Hyperkalemia
Severe hyperkalemia is the most fatal among all electrolyte abnormalities and is a medical emergency. Overall prognosis of hyperkalemia depends on the potassium level, efficacy of therapy, and comorbidities associated with the hyperkalemia. The presence of diabetic ketoacidosis and renal failure as the cause of the hyperkalemia often confer a poor prognosis.
