Left Anterior Fascicular Block (LAFB)
Left Anterior Fascicular Block occurs when the sinus impulse is delayed or interrupted within the left anterior fascicle. LAFB is the most common intraventricular conduction abnormality because the left anterior fascicle is a long and thin structure that is more delicate and more vulnerable to injury than the rest of the conduction system.
Electrocardiogram findings
LAFB alters the electrocardiogram (ECG) by abnormally shifting the axis of the QRS complex to the left of –30°. The most important leads in detecting the abnormal left axis deviation are leads II and aVL.
Lead II: This is the most important lead in suspecting that Left Anterior Fascicular Block is present. In lead II, the QRS complex is negative with an rS configuration (r wave is smaller than the S wave). Leads III and aVF will also show an rS pattern.
Lead aVL: A tall R wave in lead I (Rs complex) and a qR pattern in aVL will confirm that the axis has shifted to the left.
In LAFB, the right ventricle continues to be supplied by the right bundle branch, and the left ventricle continues to be supplied by the left posterior fascicle. Therefore, activation of both ventricles remains synchronous and the duration of the QRS complex is not increased. It normally remains at 0.08 to 0.10 seconds.
The ECG findings of Left Anterior Fascicular Block are shown in Figures 9.3 and 9.4.
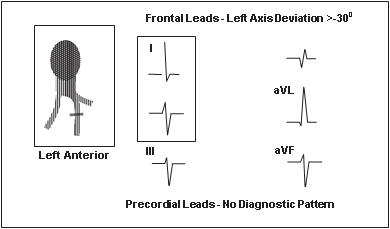
Figure 9.3: Left Anterior Fascicular Block. The hallmark of LAFB is the presence of left axis deviation >–30° with rS complexes in leads II, III, and aVF and tall R waves in leads I and aVL. Briefly, LAFB should always be suspected when there is negative or rS complex in lead II with a tall R wave in lead I (the essential leads are framed).
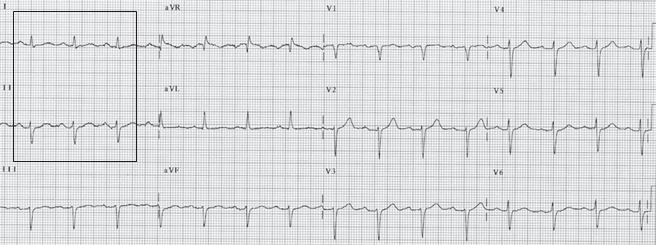
Figure 9.4: Left Anterior Fascicular Block. Twelve-lead electrocardiogram showing left anterior fascicular block (LAFB). The axis of the QRS complex is –60°. LAFB should always be suspected when a tall R wave is present in lead I and deep S wave is present in lead II (the leads are framed). The QRS complexes remain normal in duration. The precordial leads are not helpful in establishing the diagnosis, although poor R wave progression is usually present. The changes in the precordial leads are due to extreme deviation of the electrical axis superiorly. These changes may disappear if the leads are positioned two intercostal spaces higher than the standard location.
Common mistakes in left anterior fascicular block
LAFB mistaken for anterior infarct: Left Anterior Fascicular Block may cause small q waves in V2 and in V3, which can be mistaken for anteroseptal infarct (Fig. 9.5). These micro–q waves may become more exaggerated if V1 and V2 are inadvertently positioned at a higher location on the patient’s chest (at the 2nd rather than the 4th intercostal space).
LAFB mistaken for inferior infarct: LAFB may be confused with inferior myocardial infarction (MI) because both can shift the QRS axis to the left of –30°. However, inferior MI will show initial q waves in leads II, III, and aVF (Fig. 9.6), whereas the QRS complex in LAFB start with a small r wave in II, III, and aVF (Fig. 9.5).
LAFB and inferior MI: LAFB and inferior MI may be difficult to recognize when they occur together unless the leads are recorded simultaneously (Fig. 9.7A).
LAFB: For LAFB to be present, (1) the axis of the QRS complex should exceed –30°, (2) both aVR and aVL should end with R waves, and (3) the peak of the R wave in aVL should occur earlier than the peak of the R wave in aVR (Fig. 9.7B).
LAFB + inferior MI: When LAFB is associated with inferior MI, a q wave in lead II should be present (Fig. 9.8A) in addition to criteria 1, 2, and 3 for LAFB listed previously (Fig. 9.8B).
ECG of Left Anterior Fascicular Block
Frontal or limb leads:
Left axis deviation >–30° (rS complexes in II, III, and aVF and qR in I and aVL).
Normal QRS duration.
The horizontal or precordial leads are not needed for the diagnosis of LAFB.
Mechanism
- The left anterior fascicle activates the anterior and superior portions of the left ventricle. When there is Left Anterior Fascicular Block, the area supplied by the left anterior fascicle is the last to be activated. This causes the axis of the QRS complex to shift superiorly and to the left. The hallmark of LAFB is a shift in the QRS axis to the left of –30°. Although an axis of ≥–45° is the traditional criteria used in the diagnosis of LAFB, a QRS axis >–30° is accepted as LAFB.
- The QRS complex is not widened when there is LAFB because the left ventricle has two overlapping sets of Purkinje fibres: one from the left anterior fascicle and the other from the left posterior fascicle. When there is LAFB, the left ventricle is activated by the left posterior fascicle and the right ventricle by the right bundle branch, thus both ventricles remain synchronously activated. If there is any increased duration of the QRS complex, it will be minimal and should not exceed 0.01 to 0.02 seconds above baseline. Thus, the total duration of the QRS complex will remain within 0.10 seconds unless there is MI or left ventricular hypertrophy.
- In LAFB, the left ventricle is initially activated by the left posterior fascicle. Thus, the initial QRS vector is directed inferiorly and to the right, often causing q waves in V2 and V3. This becomes exaggerated if the electrodes are positioned higher on the chest or if the heart is oriented vertically.
Left posterior Fascicular Block
Frontal leads:
Axis: Right axis deviation >900. Other causes are excluded.
Lead I: rS complex
Lead aVF: Tall R in aVF and lead III with qR pattern The duration of the QRS complex remains normal
Precordial leads: No diagnostic changes
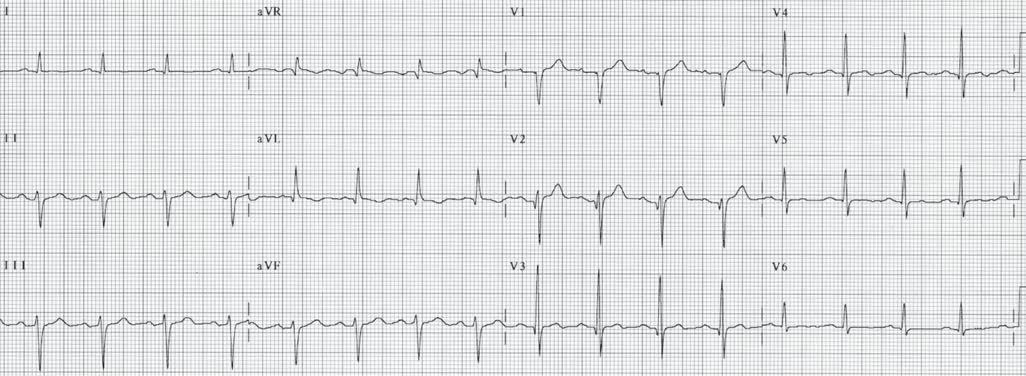
Figure 9.5: Left Anterior Fascicular Block. Left anterior fascicular block can cause small q waves in V2 and V3, which can be mistaken for anterior myocardial infarction. These micro–q waves become more pronounced if leads V1 to V3 are placed higher than the standard location and the patient is in a sitting positionwhen the electrocardiogram isrecorded.
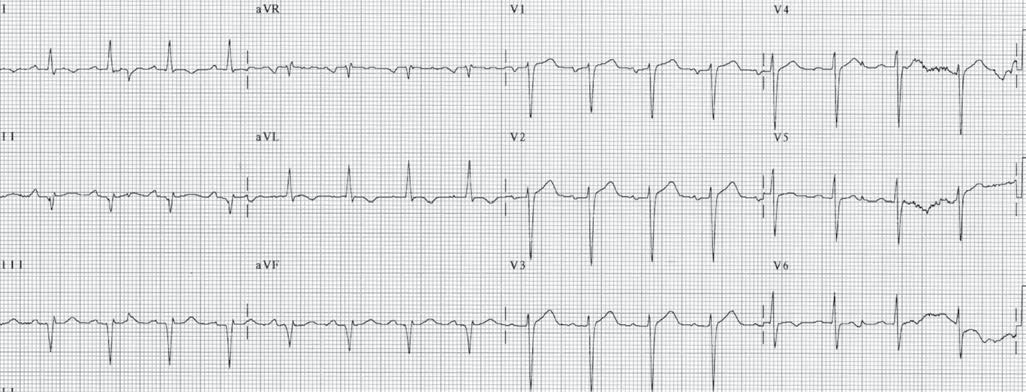
Figure 9.6: Inferior Myocardial Infarction. Left anterior fascicular block should not be confused with inferior myocardial infarction (MI). In inferior MI, leads II, III, and aVF start with a q wave as shown here, rather than with a small r.
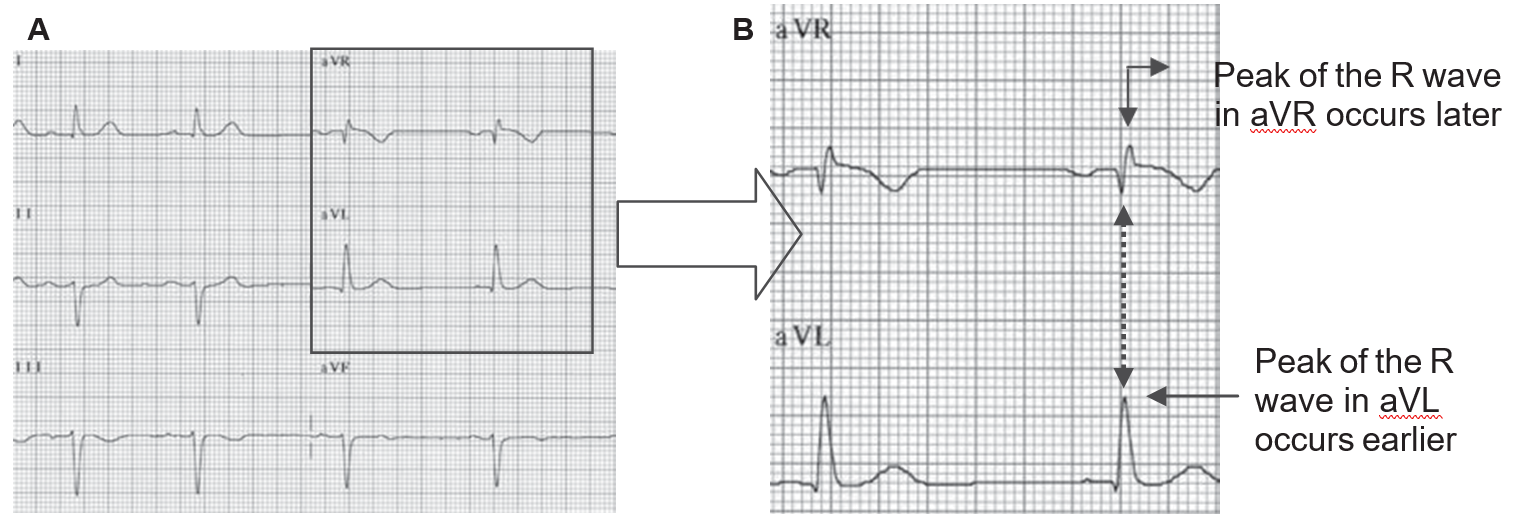
Figure 9.7: Left Anterior Fascicular Block. When leads aVR and aVL are simultaneously recorded (A), left anterior fascicular block is present when there is left axis deviation >–30° and aVR and aVL both terminate with an R wave. (B) Magnified to show that the peak of the R wave in aVL occurs earlier than the peak of the R wave in aVR.
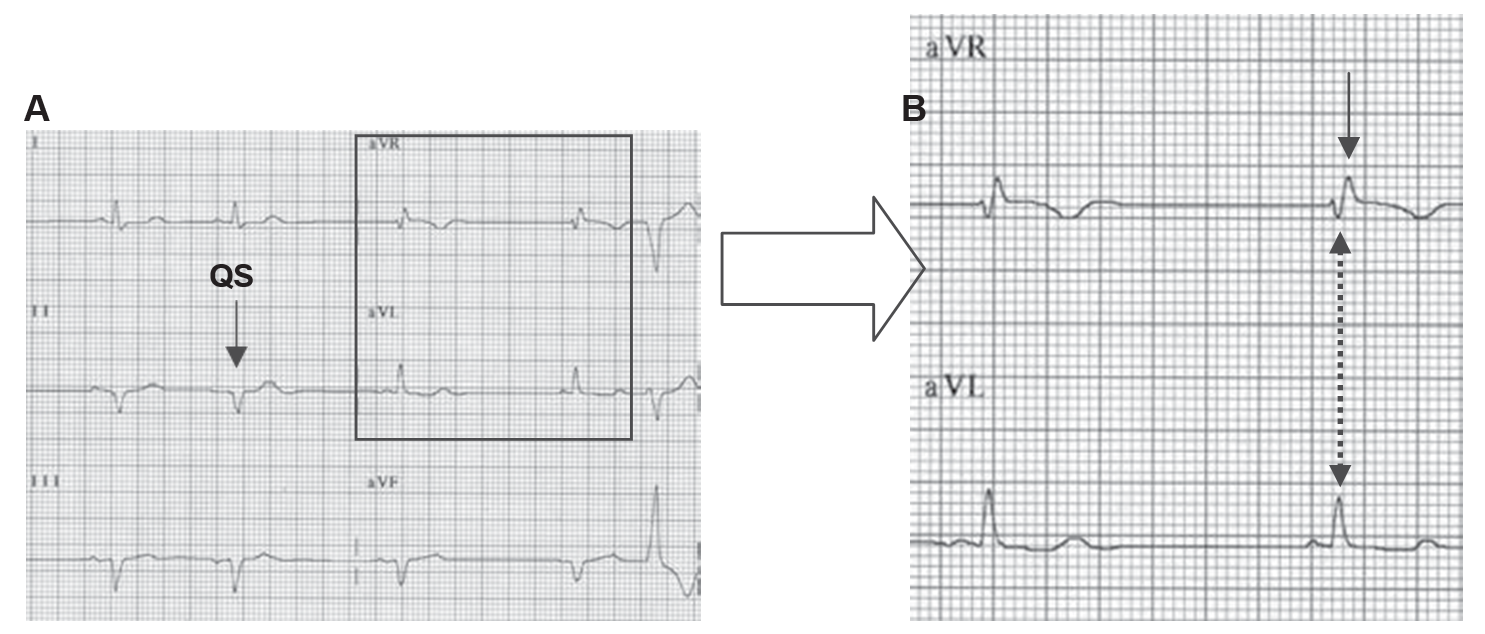 Figure 9.8: Left Anterior Fascicular Block with Inferior MI. (A) Leads aVR and aVL are recorded simultaneously and are magnified in (B). Note that the terminal R wave in aVR (arrow) occurs later than the terminal R wave in aVL, consistent with left anterior fascicular block. In addition, q waves (QS) are present in lead II (A), consistent with inferior myocardial infarction.
Figure 9.8: Left Anterior Fascicular Block with Inferior MI. (A) Leads aVR and aVL are recorded simultaneously and are magnified in (B). Note that the terminal R wave in aVR (arrow) occurs later than the terminal R wave in aVL, consistent with left anterior fascicular block. In addition, q waves (QS) are present in lead II (A), consistent with inferior myocardial infarction.
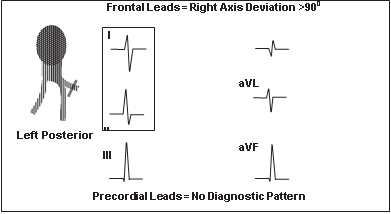
Figure 9.9: Left Posterior Fascicular Block. The most important feature of left posterior fascicular block (LPFB) is the presence of right axis deviation >90°. The diagnosis should be considered only after chronic obstructive pulmonary disease and other causes of right ventricular hypertrophy are excluded. The presence of LPFB is suspected when deep S wave is present in lead I (rS complex) and tall R wave (Rs complex) is present in lead II (the leads are framed).
Clinical Significance
The left anterior fascicle is a long and thin structure that terminates into a network of Purkinje fibres at the base of the anterior papillary muscle. It courses subendocardially in the direction of the outflow tract of the left ventricle, and thus is subject to higher intraventricular pressure than the rest of the conduction system. Because of its structure and location, LAFB is the most common intraventricular conduction abnormality.
LAFB is a common cause of left axis deviation and should be considered immediately when left axis deviation exceeds –30°. LAFB may be difficult to recognize when combined with inferior MI because both can cause left axis deviation.
LAFB: In LAFB, the QRS axis is >–30° and leads II, III, and aVF start with small r waves. The terminal QRS vector loop in the frontal plane is directed superiorly and leftward in a counterclockwise direction. Thus, the peak of the R in aVL occurs earlier than the peak of the R in aVR.
Inferior MI: In inferior MI, leads II, III, and aVF start with q waves.
LAFB and inferior MI: There is LAFB if the QRS axis is >–30°, terminal R waves are present in aVR and aVL and the peak of the R wave in aVL occurs earlier than the peak of the R wave in aVR. If any q wave is present in lead II, inferior MI is also present.
LAFB is commonly the result of hypertension, ischemic heart disease, cardiomyopathy, aortic valve disease, and sclerosis or fibrosis of the conduction system. Left ventricular hypertrophy is commonly associated with LAFB. Conversely, LAFB can augment the tall R waves in aVL, which can mimic left ventricular hypertrophy. In children, left axis deviation of ≥–30° is abnormal and is usually due to primum atrial septal defect.
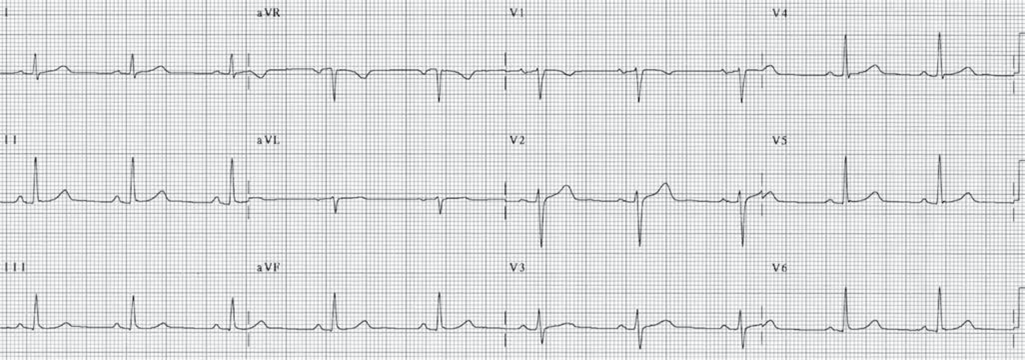
Figure 9.10: Normal Electrocardiogram. The QRS complexes are not widened, with normal axis of approximately 75°.
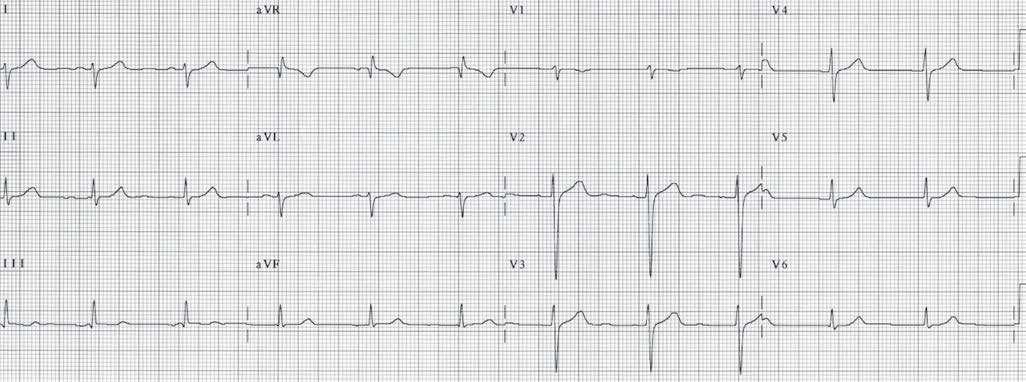
Figure 9.11: Left Posterior Fascicular Block. Twelve-lead electrocardiogram showing left posterior fascicular block (LPFB). The QRS complexes are not widened and the axis is shifted to +120°. Before LPFB is diagnosed, other causes of right axis deviation should first be excluded.
Treatment and Prognosis
- LAFB does not require any treatment. Therapy is directed to the underlying cause of the LAFB.
- The prognosis of LAFB depends on the underlying cause. If this is the only conduction abnormality and no associated cardiac disease is present, LAFB is generally benign.
