Definition:
Failure to capture means when the pacemaker initiates a stimulus, but it fails to depolarise the myocardium.
It is depicted on ECG by the presence of spikes of pacemaker but there is no associated depolarisation of the concerned chamber.
Causes of failure to capture are:
- Depletion of battry,
- Failure of circuit,
- Dislodgement of lead,
- Elevated threshold of the myocardium because of fibrosis of other cardiac diseases,
- Metabolic abnormalities like electrolyte imbalance and,
- Drugs like flecainide and amiodaroine.
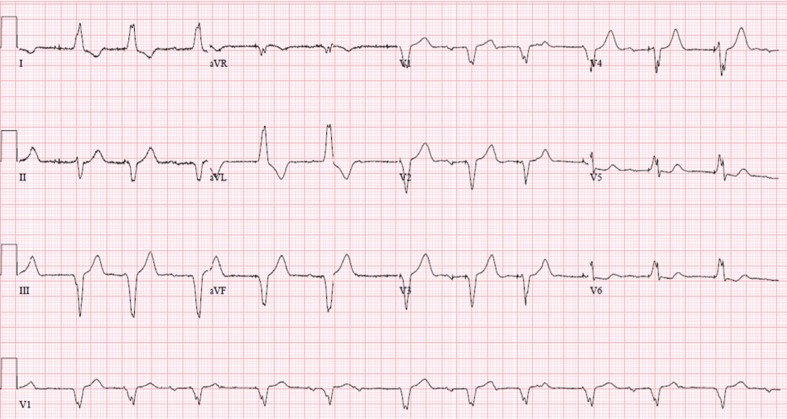
This ECG shows:
- Wide Complex Tachycardia
- QRS duration: 240ms
- Hear Rate: 115 bpm
- Group beating can be seen.
Cause: Intermittent Failure to Capture.
If we carefully see lead V1, we can see progressive widening of QRS.
But, at the same time we can see that P waves are preceded by QRS complex every time. What could be the reason?
This is rate-dependent widening of QRS also known as use-dependent widening of QRS.
It is classically seen in Flecainide treated patients.
Flecainide is a class 1c anti-arrhythmic agent.
During the refractory period of the previous beat, if ventricular pacing occurs, it results in failure to capture.
It is also known as functional non- capture.
Failure of Capture in Acute Settings
It is well known that acute failure to capture is mostly caused by lead dislodgement.
It occurs within hours to days of the procedure.
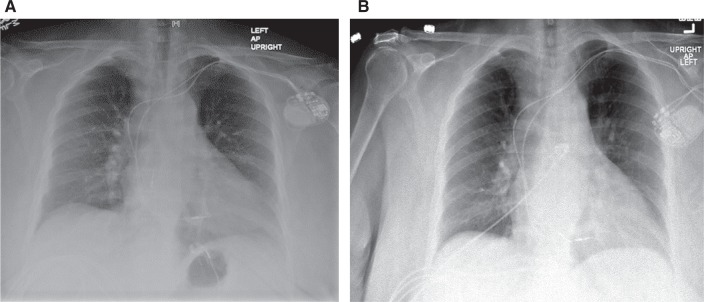
We can see this X- Ray images before and after dislodgement of the lead. The time interval between the two X- Ray films is a few days.
That is why, X- Rays play an important role in assessing lead position at different times after the procedure.
In ECG we can see the changes that were shown in Figure 1 of this article.
There can be failure to capture or there can be capture of some totally different chamber.
Treatment in such a case is by repositioning the lead in the concerned chamber.
Other causes of failure to capture are:
- Metabolic or respiratory Acidosis.
- Myocardial infarction on ischaemia.
- Use of anti- arrhythmic drugs like flecainide, as is discussed in detail in this article.
- But these causes are not that common and are relatively rare.
Failure of Capture in Chronic Settings
Here, the definition chronic means months to years after pacemaker insertion.
The underlying pathologies as to why there was the need for pacemaker insertion are eventually the underlying pathologies for a failure to capture.
Here what happens is that there is progressive increase in threshold to pace the myocardial tissue because of the reasons listed below.
Overtime the risk factors and pathologies can end up into:
- Cardiomyopathy
- Cardiac fibrosis of muscle tissue
- Inadvertent use of medications
- Metabolic disturbance like metabolic acidosis and electrolyte imbalances
- Lead fracture
- Exit block
Treatment:
- Eliminating cause
- Stopping the implicated drugs
- Repositioning of the leads
- Increasing the pacing voltage to achieve required stimulus until the underlying causes can be eliminated.
Cardiac causes of chronic failure to capture
Fibrosis is the major chronic cause of chronic failure to capture. Why fibrosis occurs? Here are a few reasons to that:
Inflammation from lead insertion site which can eventually cause failure of capture after a long time of the procedure.
Now-a-days, the leads have zotarolimus eluting tips or some steroid-eluting tips. These drugs have a well-known side effect of causing fibrosis.
Cardiomyopathy, especially restrictive cardiomyopathy at the first place, before insertion of pacemaker can be a cause of failure to capture because restrictive cardiomyopathy is itself a form of fibrosis.
Previous or a few days old myocardial infarction leaving behind the scar tissue (fibrosis) can failure of transmission of impulse and cause chronic failure to capture.
Treatment of fibrosis in failure to capture:
- If fibrosis is local at the insertion site of the tip of the pacemaker, the lead can be repositioned in order to be kept at some fresh location from where the impulse can be conducted in a correct manner.
- If there is lead fracture, total new replacement of lead with a revised procedure is the treatment of choice.
Case presentation on intermittent failure to capture
82 years old female with a history of hypertension and paroxysmal atrial fibrillation and sick sinus syndrome had undergone a procedure for dual- chamber pacemaker insertion three years ago.
She was referred to us for evaluation of wide complex tachycardia and a heart rate of 115 bpm.
She was taking following medications:
- Candesartan 32 mg OD
- Hydrochlorthiazide 12.5 mg OD
- Flecainide 100 mg OD
- Metoprolol 25 mg BD
- Amiodarone 200 mg OD.
Lab tests showed findings of Acute Kidney Injury with following features:
- Bicarbonate 12 mmol/L
- BUN 63 mg/dL
- Creatinine 2.5 mg/dL
Her ECG is shown in the image below:

The image shows an ECG of acute intermittent failure to capture.
What could be the possible mechanism?
Explanation:
Acute kidney injury, repeated episodes of vomiting, use of hydrochlorthiazide and amiodarone (intravascular volume depletion) raises the suspicion of toxicity of the drug which is very infamous for narrow therapeutic index and is being used in this patient i.e., flecainide (class 1c anti-arrhythmic agent)
How was she treated?
- We discontinued amiodarone and flecainide.
- Mode of pacemaker was changed.
- Rate of pacemaker was changed and was reduced to 70 bpm.
- Patient was rehydrated with intravascular fluids.
- All the metabolic abnormalities were corrected within a period of 48 hours.
- Her kidney injury resolved and cardiac rhythm was stabilised back to normal.
- The changes are seen clearly in Figure 3B and a Figure 3A (baseline ECG) is also shown here for comparison.
Figure 4A shows:
- Wide complex tachycardia (QRS= 240ms)
- Heart Rate= 115 bpm
- Intermittent failure with group beating.
- Rate-dependent QRS widening
Cause: Flecainide toxicity
Differential diagnosis: Sinus tachycardia with ventricular pacing.
Figure 4B shows and ECG with normal heart rate and rhythm with normal pacing. It was recorded 48 hours after the admission of the patient.
