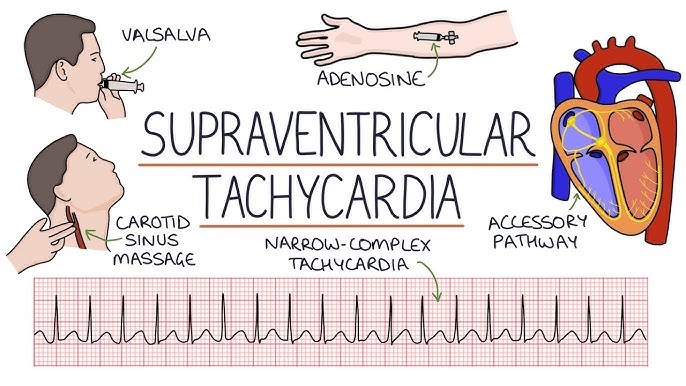
Supraventricular Tachycardia Introduction
Tachycardia refers to a heart rate >100 beats per minute (bpm). The tachycardia may be supraventricular or ventricular depending on the origin of the arrhythmia.
Supraventricular Tachycardia (SVT): If the tachycardia originates above the bifurcation of the bundle of His, usually in the atria or atrioventricular (AV) junction, the tachycardia is supraventricular.
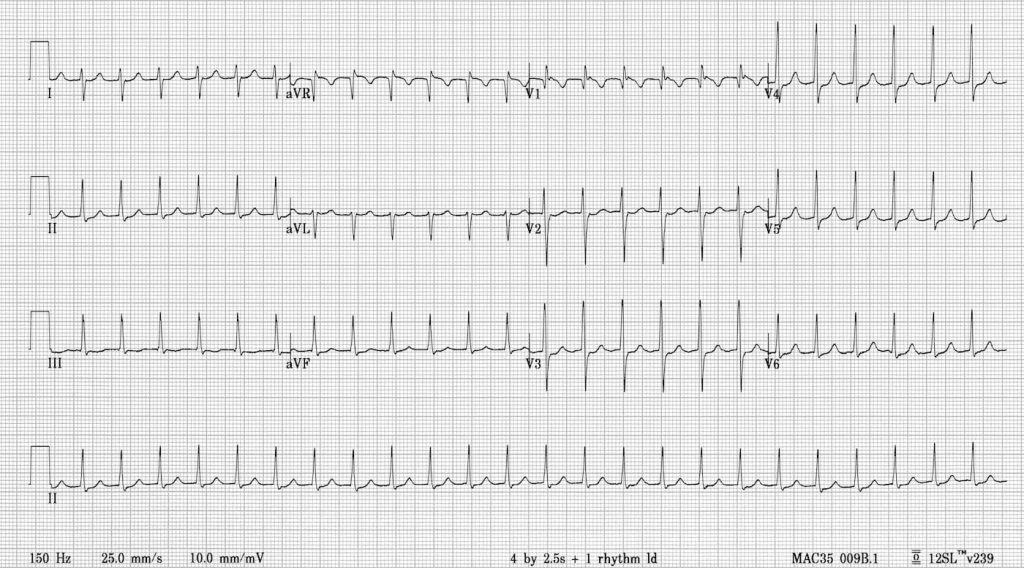
Supraventricular impulses follow the normal AV conduction system, activate the ventricles synchronously and will have narrow QRS complexes measuring <120 milliseconds. The QRS may be wide if there is pre-existent bundle branch block, ventricular aberration, or the impulse is conducted through a bypass tract.
Ventricular tachycardia (VT): If the tachycardia originates below the bifurcation of the bundle of His, the tachycardia is ventricular. The impulse will spread to the ventricles outside the nor- mal AV conduction system. Activation of the ventricles will not be synchronous resulting in wide QRS complexes measuring ≥120 milliseconds.
There are other types of tachycardias with narrow QRS complexes other than SVT. These include sinus tachycardia, atrial flutter, and atrial fibrillation. These tachycardias should be distinguished from each other be- cause the treatment of these various arrhythmias is different.
Sinus tachycardia: Sinus tachycardia implies that the rhythm originates from the sinus node with a rate that exceeds 100 bpm. Sinus tachycardia is a normal finding, which is usually an appropriate response to a physiologic or pathologic condition.
Atrial flutter: The diagnosis of atrial flutter is based on the presence of a very regular atrial rate of 300 ± 50 bpm.
Atrial fibrillation: The diagnosis of atrial fibrillation is based on an atrial rate of 400 ± 50 bpm with characteristic baseline fibrillatory pattern and irregularly irregular R-R intervals. This will also be discussed separately.
Supraventricular Tachycardia (SVT): SVT is a narrow complex tachycardia originating outside the sinus node but above the bifurcation of the bundle of His, with a rate that exceeds 100 bpm. Several types of SVT are present and are classified according to three general mechanisms: reentry, enhanced automaticity, and triggered activity.
| Narrow Complex Tachycardia | ||||
| Sinus Tachycardia | SVT | Atrial Flutter | Atrial Fibrillation | |
| Sinus Rate >100 | Reentrant AVNRT AVRT Intraatrial Sinoatrial | Automatic Atrial >Focal or unifocal >Multifocal Junctional >Paroxysmal >Nonparoxysmal | Atrial Rate 300 ± 50 | Atrial Rate 400 ± 50 |
| Atrial Rate 200 ± 50 | ||||
| Table shows the different tachycardias that can result in narrow QRS complexes. Generally, the atrial rate of atrial fibrillation is 400 ± 50 bpm, for atrial flutter 300 ± 50 bpm, for SVT approximately 200 ± 50 and for sinus tachycardia >100 bpm. AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; SVT, supraventricular tachycardia. | ||||
- Re-entry: SVT due to re-entry is an abnormality in the propagation of the electrical impulse resulting from the presence of two separate pathways with different electrophysiologic properties.
- Enhanced automaticity: This is an abnormality in initiation rather than conduction of the electrical impulse. Some cells in the atria or AV junction may exhibit phase 4 diastolic depolarization and may spontaneously discharge faster than that of the sinus node if the discharge rate is enhanced.
- Triggered activity: This is also an abnormality in initiation of the electrical impulse resulting from occurrence of afterdepolarizations. Afterdepolarizations are secondary depolarizations that are triggered by the initial impulse. The afterdepolarization does not always reach threshold potential, but when it does, it may be followed by repetitive firing of the membrane voltage. Triggered activity is usually seen in association with digitalis toxicity, calcium ex- cess, or increased catecholamines. SVT from re-entry usually occurs in normal individuals without evidence of structural cardiac disease. SVT from enhanced automaticity may occur in normal individuals, although they are more frequently associated with structural cardiac diseases, abnormalities in electrolytes and blood gasses, or use of pharmacologic agents. SVT from triggered activity usually occurs with digitalis ex- cess or after cardiac surgery.
| Differences between SVT because of Reentry, Enhanced Automaticity, and Triggered Activity | |||
| Reentry | Enhanced Automaticity | Triggered Activity | |
| Mechanism | This is an abnormality in impulse conduction. A reentrant circuit is present. | This is an abnormality in impulse initiation. Cells with automatic properties become the dominant pacemaker. | Early or late after- depolarizations are present. |
| Initiation | Initiated by premature impulses or by rapid pacing. | Initiated by increased firing rate of automatic cells in the atria or AV junction. | Initiation is not well defined. |
| Termination | Terminated by vagal maneuvers, AV nodal blockers, ectopic impulses, overdrive pacing, or electrical cardioversion. | Not usually terminated by vagal maneuvers, AV nodal blockers, ectopic impulses, overdrive pacing or electrical cardioversion. | May be terminated by premature impulses, overdrive pacing, or electrical cardioversion. |
| Underlying Condition | Frequently seen in structurally normal hearts. | Frequently seen in patients with metabolic or pulmonary disorders or patients on adrenergic drugs, caffeine, theophylline, or other agents. | Frequently seen in patients with digitalis toxicity or postcardiac surgery. |
| Examples of SVT | AV nodal reentryAV reentrySinoatrial reentryIntraatrial reentry | AT O Focal AT O Multifocal AT Junctional tachycardia O Focal or paroxysmal O Nonparoxysmal | Atrial tachycardia with 2:1 AV blockNonparoxysmal junctional tachycardia |
| SVT, supraventricular tachycardia; AT, atrial tachycardia; AV, atrioventricular. | |||
Treatment of Supraventricular Tachycardia
Different causes of Supraventricular Tachycardia have different treatment therapies.
There is a proper algorithm which has been developed in order to treat Suprsventricular Tachycardia in minimum amount of time and avoiding unnecessary steps at the same time.
Here is an example of algorithm which is used in the treatment of hemodynamically stable supraventricular tachycardia(AVNRT). Individual treatment details of other supraventricular tachycardias will be addressed in their respective articles.