Overview of Hypokalemia
Hypokalemia is defined as the presence of serum potassium that is lower than normal. The normal value for serum potassium is 3.3 to 5.3 mmol/L.
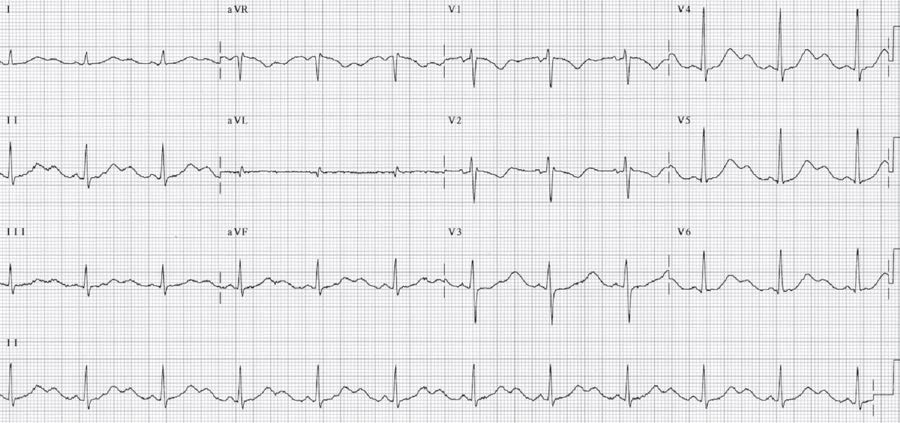
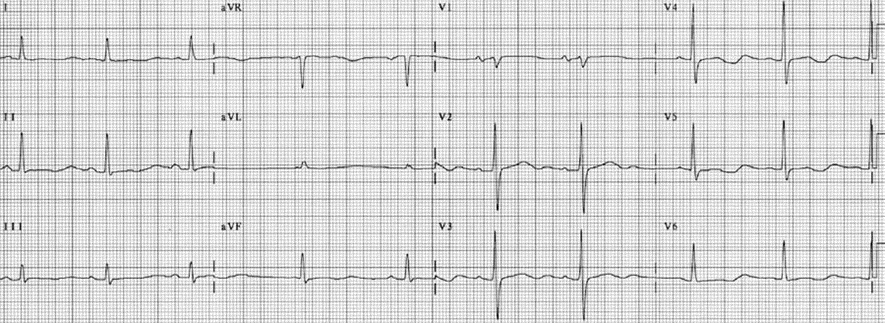
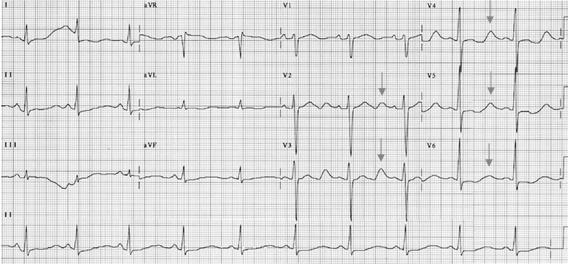
The most important ECG finding in hypokalemia is the presence of prominent U waves. As the hypokalemia becomes more profound, the amplitude of the T wave becomes lower as the size of the U wave becomes larger until both T and U waves bond together and become indistinguishable (Figs. 1 and 2).

Normal U wave: The U wave follows the T wave and is the last component of ventricular repolarization. The normal U wave is small measuring less than a quarter of the size of the T wave. The exact origin of the normal U wave is uncertain but is most probably from the repolarization of the Purkinje fibers.
Hypokalemic U wave: The U wave in hypokalemia is large and pathologic. It is much larger than the T wave and its origin is not the same as that of the normal U wave. It has been shown that in hypokalemia, the normal T wave becomes interrupted, splitting into two components. The T wave represents the first component and the U wave the second component. Thus, the Q-U interval truly represents the actual QT interval and is prolonged. The QT interval represents only the first component of the split T wave, and is equal to or even shorter than the normal QT interval (Figs. 3-6).
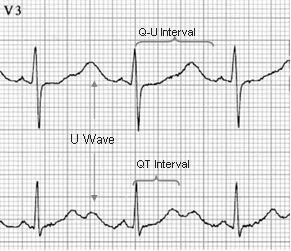
Figure 3: The QT and the Q-U Interval in Hypokalemia. Lead V3 and lead II were simultaneously recorded. In lead II, the U waves are separately inscribed from the T waves and the two humps resemble the back of a camel. If the QT interval is measured in lead II, the QT interval is short since it represents only the first component of a split T wave. It does not represent the real QT interval. In V3, the U waves are very prominent and can not be separated from the T wave. This QU interval represents the actual QT interval and is prolonged. The 12-lead electrocardiogram is shown in Figure 2.

ECG Findings of Hypokalemia
- Prominent U waves
- Nonspecific ST depression and T-wave flattening as the U wave becomes more prominent
- Prolongation of the QU interval
- Fusion of the T and U waves
- Ventricular arrhythmias, especially torsade de pointes
Mechanism
- The ratio between intracellular and extracellular potassium determines the resting potential of a cell, which is normally –90 mV. When there is hypokalemia, extracellular potassium is decreased and the ratio between intracellular and extracellular potassium becomes higher. Thus, the cells become more negative than –90 mV and the resting potential is hyperpolarized. This will cause lengthening of the duration of the action potential resulting in a longer QT interval in the surface ECG. This will increase the frequency of ventricular arrhythmias especially torsade de pointes.
- The ECG hallmark of hypokalemia is the presence of prominent U waves and prolongation of the QU interval. As hypokalemia worsens, the T wave flattens, a U wave emerges, and a seesaw effect between the amplitude of the T and U wave occurs. As the U wave grows larger, the T wave becomes smaller. Merging of the T and U waves eventually occur; thus, the T and U waves become indistinguishable from one another.
- In hypokalemia, phase 3 of the transmembrane action potential is less steep causing a small or attenuated intramyocardial voltage gradient, resulting in low T waves. This is opposite to that of hyperkalemia, where phase 3 has a steeper slope, which translates into a higher intramyocardial voltage gradient, resulting in T waves that are taller and more peaked.
- According to Yan et al., the mechanism of a pathologic U wave resulting from hypokalemia is different from the mechanism of a normal U wave. When hypokalemia is present, the abnormal T-U complex has been shown to be due to splitting of the ascending limb of the normal T wave into two components. The first component of the split T wave is the original T wave and the other component becomes a separate U wave, which is actually the other half of the split T wave. If only the QT interval is measured, which represents only the first component of the bifid T wave, the QT interval is equal to or even shorter than the normal QT interval. Thus, in hypokalemia, measurement of the true QT interval should include the U wave and is measured as the QU interval.
Clinical Implications
- The normal level of potassium in the blood is 3.3 to 5.3 mmol/L. Hypokalemia refers to the presence of lower than normal potassium in the blood, which is <3.3 mmol/L.
- The normal daily intake of potassium varies from 80 to 120 mEq/day. Almost 90% of dietary potassium is excreted by the kidneys and the rest by the gastrointestinal (GI) tract.
- Hypokalemia usually occurs from potassium loss in the kidneys, frequently brought about by chronic diuretic therapy or potassium loss in the GI tract as a result of frequent vomiting, continuous gastric suction, or diarrhea.
- Hypokalemia also occurs when there is acute shift of extracellular potassium intracellularly from metabolic alkalosis or drugs such as insulin and beta agonists. Alkalosis causes extracellular potassium to move into the cell in exchange for H+, resulting in a lower level of serum potassium. Metabolic alkalosis decreases serum potassium by 0.8 mmol/L for every 0.1 unit increase in pH above normal. Acidosis causes a reverse effect with intracellular potassium moving out of the cell in exchange for H+. Thus, an acidotic patient with a normal potassium level is expected to develop hypokalemia once the acidosis is corrected.
- Symptoms of hypokalemia usually occur when significant electrolyte depletion has occurred. This is usually manifested as generalized weakness, fatigue, and paralysis.
- In patients who are being weaned off a respirator, it is important that potassium level should be checked because hypokalemia can cause muscle weakness that can result in respiratory failure. If hypokalemia is present, the electrolyte abnormality should be corrected.
- Hypokalemia can affect the muscles of the GI tract, resulting in ileus or constipation. It can also affect the muscles of the lower extremities, resulting in leg cramps and paresthesias.
- Arrhythmias including torsade de pointes and pulseless electrical activity may occur when the QT (or QU) interval is prolonged.
Treatment of Hypokalemia
- Because potassium is predominantly an intracellular ion, hypokalemia may occur even when total body potassium is normal or higher than normal. Generally, however, when hypokalemia is present and is from chronic loss of potassium, a decrease in serum potassium of 1 mmol/L is equivalent to a deficit of approximately 150 to 400 mmol of body potassium.
- Therapy of hypokalemia includes identification and correction of the underlying abnormality.
- Aggressive intravenous replacement of potassium may be associated with hyperkalemia and cardiac arrhythmias. Thus, intravenous administration of potassium is preferred when arrhythmias are present or when hypokalemia is severe (<2.5 mEq/L). Oral replacement is given if the patient is clinically stable without arrhythmias and the potassium level is ≥2.5 mmol/L because administration of potassium orally is much safer and can be given in higher doses.
- Replacement therapy of approximately 200 to 300 mmol potassium is needed to increase the serum potassium level by 1 mmol/L. However, it may take several days to correct the electrolyte abnormality because the administered potassium is also excreted in the urine. Since intravenous replacement of potassium can potentially cause cardiac arrhythmias, the AHA guidelines recommend the following:
- The maximum infusion of potassium should not exceed 10 to 20 mmol/hour and should be infused under continuous cardiac monitoring.
- Potassium when given >20 mmol/hour should be infused with a central line. This concentration of potassium may be painful when given IV because it may cause sclerosis of the veins. The tip of the central catheter should not extend to the right atrium or ventricle because this may cause local hyperkalemia.
- If severe life-threatening arrhythmias are present and a more rapid infusion is necessary, an initial infusion of 10 mmol IV is given over 5 minutes and repeated once if necessary.
- Potassium is preferably mixed with non-glucose solutions to prevent insulin secretion, which can shift potassium intracellularly.
- Hypokalemia is usually associated with other electrolyte abnormalities, especially hypomagnesemia. When there is hypomagnesemia, it might be difficult to correct the potassium deficiency because magnesium is necessary for the movement of electrolytes in and out of the cell including potassium; therefore, correcting both electrolyte abnormality should be done simultaneously.
- The use of potassium sparing diuretics should be considered in hypokalemic patients requiring long term diuretic therapy.
Prognosis
- Hypokalemia can cause ventricular arrhythmias and may be fatal if left uncorrected. It is usually from aggressive use of diuretics or gastrointestinal losses.
- Unlike patients with hyperkalemia, the renal function in hypokalemic patients is usually preserved. After the hypokalemia is corrected, prognosis will depend on the underlying cause.
