Left Posterior Fascicular Block
- Left posterior fascicular block: LPFB occurs when conduction across the left posterior fascicle is delayed or interrupted. It is the least common among all intraventricular conduction abnormalities.
- ECG Findings: The hallmark of LPFB is a shift in the electrical axis of the QRS complex to the right of 90° (Fig. 9.9). Because LPFB is uncommon, other more common causes of right axis deviation should first be excluded before LPFB is diagnosed. The QRS complexes are not widened because the left ventricle continues to be activated by the left anterior fascicle. A normal ECG is shown in Fig. 9.10. For comparison, the ECG of LPFB is shown in Fig. 9.11.
Common mistakes in Left Posterior Fascicular Block
- Right ventricular hypertrophy mistaken for LPFB: LPFB is relatively uncommon and is considered a diagnosis of exclusion. Other causes of right axis deviation, such as right ventricular hypertrophy or pulmonary disease, should first be excluded before the diagnosis of LPFB is considered (Figs. 9.12 and 9.13). This contrasts with LAFB, where the diagnosis is considered immediately when the axis is >–30°.
- Lateral MI mistaken for LPFB: High lateral MI can cause right axis deviation >90° and can be mistaken for LPFB. In LPFB, rS complexes are present in I and aVL (Fig. 9.11). In lateral MI, QS complexes are present in these leads (Fig. 9.14).
ECG of (LPFB)Left Posterior Fascicular Block
Frontal or limb leads:
Right axis deviation >90° with negative or rS complex in I and aVL and qR in III and aVF.
The QRS complexes are not widened.
Other causes of right axis deviation have been excluded.
Horizontal or precordial leads:
The precordial leads are not necessary in the diagnosis of Left Posterior Fascicular Block.
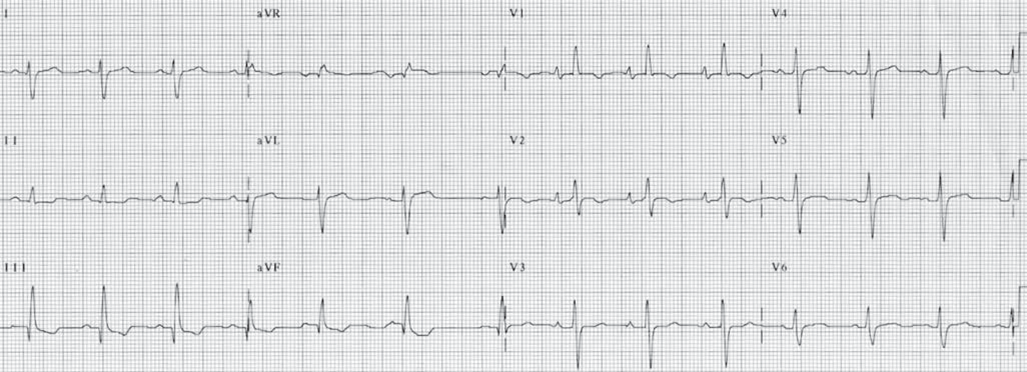
Figure 9.12: Right Ventricular Hypertrophy. The frontal leads show all features of left posterior fascicular block. However, tall R waves are present in V1, suggesting right ventricular hypertrophy and not Left Posterior Fascicular Block.
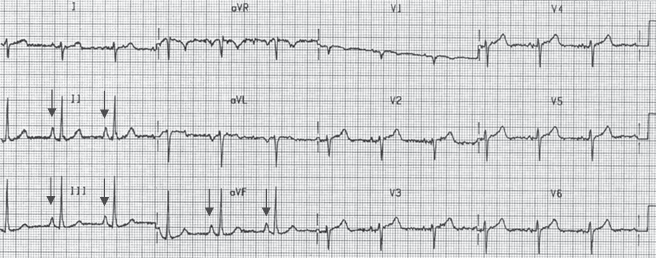
Figure 9.13: Right Ventricular Hypertrophy. There is right atrial enlargement with peaked P waves in leads II, III, and aVF (arrows). There is clockwise rotation of the QRS complexes in the precordial leads. This electrocardiogram is consistent with right ventricular hypertrophy and not left posterior fascicular block.
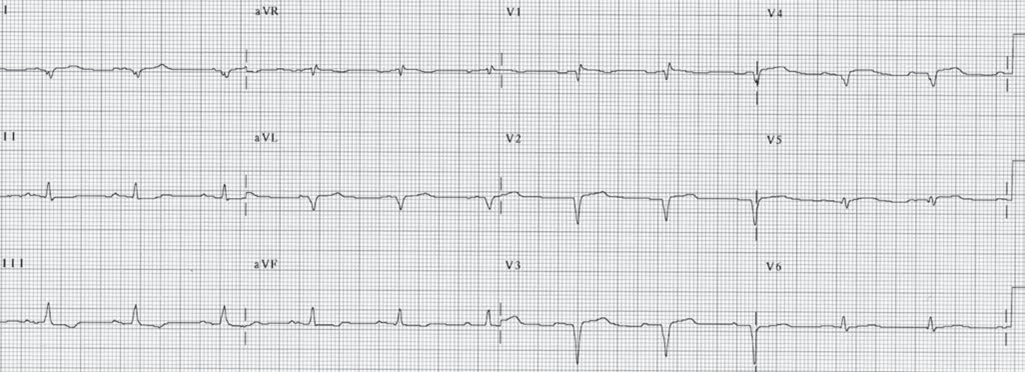
Figure 9.14: Lateral Myocardial Infarction. Lateral myocardial infarction (MI) with QS complexes in I and aVL can be mistaken for left posterior fascicular block as shown here. In LPFB, leads I and aVL have rS complexes, whereas in lateral MI, these leads start with q waves. Q waves are also present in V1 to V4 because of anterior MI.
Mechanism of Left Posterior Fascicular Block
The left posterior fascicle activates the posteroinferior left ventricular free wall, which is to the right and inferior to that activated by the left anterior fascicle. This portion of the left ventricle is the last to be activated when there is Left Posterior Fascicular Block, thus causing the axis of the QRS complex to shift inferiorly and to the right. While a QRS axis ≥100° is traditionally used to identify LPFB, a QRS axis >90° is generally accepted as LPFB.
The QRS complex is not widened when there is Left Posterior Fascicular Block because the left ventricle continues to be activated by the left anterior fascicle and the right ventricle by the right bundle branch, resulting in synchronous activation of both ventricles.
Clinical Significance of Left Posterior Fascicular Block
LPFB is a diagnosis of exclusion since Left Posterior Fascicular Block is relatively uncommon. This contrasts with LAFB, in which the diagnosis is considered outright when there is left axis deviation >–30°. Before the diagnosis of Left Posterior Fascicular Block is considered, other, more common, causes of right axis deviation such as pulmonary disease and other causes of right ventricular hypertrophy should first be excluded.
In contrast to the left anterior fascicle, the left posterior fascicle has a dual blood supply, originating from the septal perforating branches of the left anterior descending coronary artery anteriorly and from the septal perforating branches of the posterior descending artery posteriorly. It is short, thick, and broad and courses along the inflow tract of the left ventricle before terminating into a network of Purkinje fibres at the base of the posteromedial papillary muscle. It is therefore protected and subjected to less intraventricular pressure compared with the left anterior fascicle. Because of its structure, location, and blood supply, Left Posterior Fascicular Block is the least common among all intraventricular conduction abnormalities.
The most important lead in recognizing Left Posterior Fascicular Block is lead I. This will show a negative or rS complex, with the S wave deeper than the size of the r wave. This is accompanied by tall R waves in leads aVF and III.
Right axis deviation due to high lateral MI can be mistaken for Left Posterior Fascicular Block. Correspondingly, LPFB can obscure the ECG changes of inferior MI.
The causes of LPFB are the same as that of LAFB and include coronary disease, hypertension, cardiomyopathy, acute myocarditis, valvular disease (especially aortic stenosis), and degenerative diseases of the conduction system.
Treatment of Left Posterior Fascicular Block
Treatment is directed toward the underlying cause of the LPFB.
Prognosis of Left Posterior Fascicular Block
Because the left posterior fascicle is the least vulnerable and the last to be involved when there is intraventricular conduction defect, LPFB seldom occurs independently and is frequently seen in combination with right bundle branch block or with LAFB. LPFB, therefore, indicates a more significant and more advanced form of conduction abnormality than LAFB. LPFB in combination with LAFB can result in left bundle branch block. The prognosis depends on the cause of the conduction abnormality.
