Basic electrocardiographic manifestation and mechanism of Left Ventricular Hypertrophy
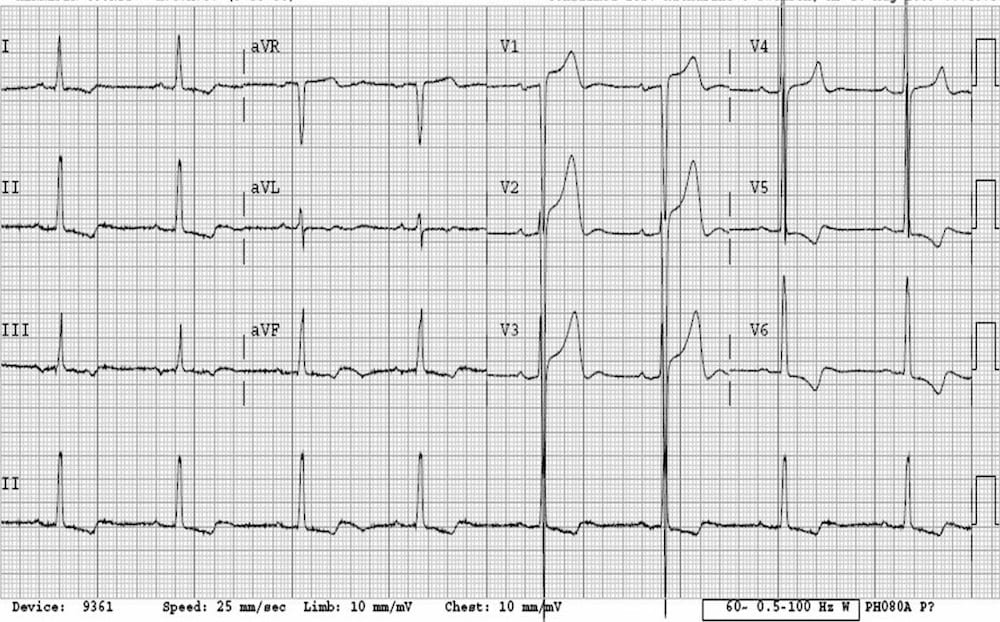
The S wave of a right-orientated lead and the R wave of a left-orientated lead represent, in effect, the resultant and dominant right-to-left QRS vector of ventricular depolarization.
These deflections constitute an indirect representation of left free-wall activation. This is due to the domination of left ventricular free-wall activation over the right ventricular free-wall activation.
Hypertrophy of the free wall of the left ventricle will result in an increased magnitude of this dominant right-toleft QRS vector, which will consequently be expressed by:
- an increase in the depth of the S wave in leads V1 and V2 and,
- an increase in the height of the R wave in leads V5 and V6.
Haemodynamic or overload concept of Left Ventricular Hypertrophy
Left ventricular hypertrophy may occur as a result of two basic haemodynamic abnormalities: systolic overload and diastolic overload.
Systolic overload is the expression of resistance to left ventricular systolic outflow and, hence, left ventricular systolic contraction.
The left ventricular compromise occurs during ventricular systole.
Systolic overload is also known as pressure overload and occurs with aortic stenosis, systemic hypertension, hypertrophic cardiomyopathy and coarctation of the aorta.
Diastolic overload is due to overfilling of the left ventricle in diastole so that the left ventricular compromise occurs during diastole. Left ventricular diastolic overload also known as volume overload occurs with mitral regurgitation and aortic regurgitation.
It also occurs with moderate to large left-toright shunts, since this will increase the volume of blood that returns to the left side of the heart, as, for example, in patent ductus arteriosus and ventricular septal defect.
These two haemodynamic disturbances gets reflected electrocardiographically by the basic abnormal QRS voltage manifestations as outlined earlier.
They are differentiated principally by certain characteristic manifestations that affect the ST segment and the T wave.
Electrocardiographic manifestations of left ventricular hypertrophy due to systolic overload
Abnormalities of the QRS complex
- Increased magnitude of the QRS deflections
- Attenuation of the small initial q wave in left-orientated leads
- An increase in left ventricular activation time
- Increase in total QRS duration
- Counterclockwise electrical rotation
Abnormalities of the ST segment and T wave
- Inversion of the U wave in left precordial leads
- Left atrial abnormality
- Abnormalities of the QRS and T wave axes
What ChatGPT says about Left Ventricular Hypertrophy?
Left ventricular hypertrophy (LVH) is a medical condition in which the muscular wall of the left ventricle, the main pumping chamber of the heart, becomes abnormally thickened or enlarged. This thickening occurs in response to increased workload or pressure on the heart, typically due to conditions that make the heart work harder to pump blood, such as high blood pressure (hypertension) or aortic valve stenosis.
The left ventricle is responsible for pumping oxygen-rich blood into the body’s main artery, the aorta, and from there, it is distributed throughout the body. When the left ventricle hypertrophies or thickens, it may not pump blood as effectively as it should. This can lead to various cardiovascular problems and increase the risk of heart-related complications, including:
- Heart Failure: The thickened heart muscle can become stiff and less able to relax and fill with blood during the diastolic phase of the cardiac cycle, which impairs the heart’s ability to pump effectively, leading to heart failure.
- Arrhythmias: LVH can disrupt the normal electrical signaling within the heart, increasing the risk of abnormal heart rhythms, such as atrial fibrillation, ventricular tachycardia, or ventricular fibrillation.
- Ischemic Heart Disease: LVH can reduce the blood supply to the heart muscle itself, leading to a condition called ischemic heart disease or coronary artery disease. This can result in chest pain (angina) and potentially lead to heart attacks.
- Stroke: LVH is associated with an increased risk of stroke, likely due to its association with high blood pressure and atrial fibrillation.
- Sudden Cardiac Death: In severe cases, LVH can increase the risk of sudden cardiac death, particularly if it is associated with certain arrhythmias.
The diagnosis of LVH is often made through various tests, including echocardiography (ultrasound of the heart), electrocardiography (ECG or EKG), and magnetic resonance imaging (MRI). The treatment of LVH typically involves managing the underlying cause, such as controlling high blood pressure or treating heart valve disorders. Lifestyle modifications, such as adopting a heart-healthy diet, exercising regularly, and quitting smoking, are also essential in managing LVH. In some cases, medications may be prescribed to reduce the workload on the heart and prevent further thickening of the left ventricle. Severe cases may require surgical interventions, such as valve replacement or correction of congenital heart defects.
It’s important for individuals with LVH to work closely with their healthcare providers to develop a treatment plan that addresses the underlying causes and reduces the risk of complications. Regular follow-up appointments and monitoring of the condition are usually necessary to ensure optimal management.
GMCMedicine further readings-
- Junior Resident Doctor Salary in India
- Basic Principles of Arrhythmogenesis
- ECG in Right Ventricular Hypertrophy
- ECG in Coronary Artery Disease
- Next Exam Pattern
External sources to read Basic Principles of ECG-