Overview of Hypocalcemia
- Hypocalcemia is defined as a calcium level below the normal range. The normal serum calcium level varies from 8.5 to 10.5 mg/dL and the normal level of ionized calcium is 4.2 to 4.8 mg/dL.
- When the level of extracellular calcium is decreased, the following ECG changes occur:
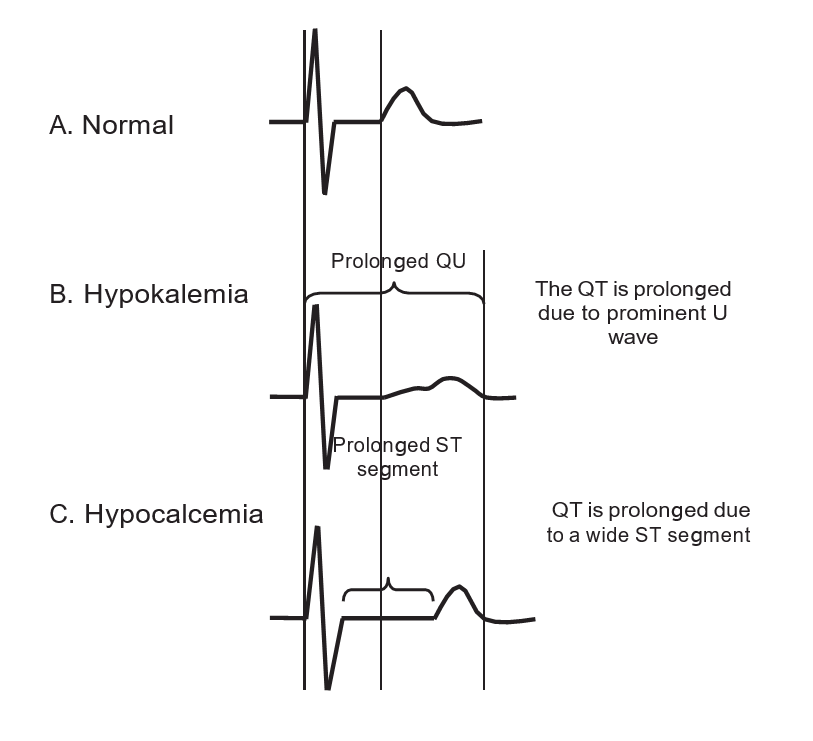
- The QT interval is prolonged. Prolongation of the QT interval is due to prolongation of phase 2 of the action potential, which corresponds to the ST segment in the ECG. Thus, prolongation of the QT interval is mainly due to prolongation of the ST segment. The T wave is not significantly affected. Terminal inversion of the T waves may occur (Figs. 1- 4).
- Heart block may occur when the hypocalcemia is more severe.
ECG Abnormalities of Hypocalcemia
- Prolonged QT interval due to lengthening of the ST segment.
- Flat ST segment and terminal T-wave inversion.
- Heart block and ventricular fibrillation when hypocalcemia is severe.
Mechanism
- Prolongation of the QT interval. Prolongation of the QT interval is due to lengthening of phase 2 of the action potential.
- Because phase 2 of the action potential corresponds to the ST segment, prolongation of the QT interval is mainly from lengthening of the JT interval, which represents the interval between the end of the QRS complex and the end of the T wave.
- Although the ST segment lengthens, the size of the T wave is not altered. This is the most diagnostic ECG abnormality associated with hypocalcemia. This is in contrast to hypokalemia where a prominent U wave is present resulting in prolongation of the QT (QU) interval.
- Other ECG findings include flat ST segment, widening of the QRS complex, and AV block. Ventricular fibrillation may occur when hypocalcemia is severe.
Clinical Implications
- Hypocalcemia refers to a low level of serum calcium below the normal range of 8.5 to 10.5 mg/dL (or 2.1 to 2.6 mmol/L). It is also defined as below the normal level of ionized calcium, which is 4.2 to 4.8 mg/dL (or <1.0 mmol/L).
- The recommended daily calcium is 1,200 mg. Hypocalcemia can occur when there is:
- Decreased intake or diminished absorption of calcium: Vitamin D is necessary for absorption of calcium in the GI tract. Vitamin D deficiency can occur in patients who are not exposed to sunlight or do not have adequate vitamin D in the diet. In chronic renal failure, there is defective hydroxylation of vitamin D to active vitamin D. Secondary increase in PTH may occur in an effort to maintain serum calcium levels.
- Parathyroid hormone deficiency: This is usually the result of inadvertent removal of the parathyroid glands during thyroid surgery. The parathyroid glands are also affected by tumor or by infiltrative disorders, such as hemochromatosis or sarcoidosis.
- Alkalosis: Metabolic or respiratory alkalosis decreases the level of ionized calcium.
- Chelation of calcium with citrate and other substances: Hypocalcemia may occur following transfusion of >6 units of citrated blood.
- Increased phosphates from acute renal failure and exogenous bicarbonates and free fatty acids during acute pancreatitis can also result in chelation of calcium.
- Signs and symptoms of hypocalcemia are dependent not only on the level of free or ionized calcium, but also on the rapidity in which calcium declines.
- In renal patients, hypocalcemia may not be clinically manifest because of coexistent acidosis, which increases the level of ionized calcium and may abruptly manifest only when the acidosis is corrected.
- Symptoms of hypocalcemia usually do not occur until the level of ionized calcium falls below 0.7 mmol/L. This includes generalized irritability, hyperreflexia, muscle cramps, tetany, carpopedal spasm, seizures, and neuromuscular excitability characterized by a positive Chvostek and Trousseau signs.
- Chvostek sign is elicited by tapping the facial nerve on the face anterior to the ear resulting in twitching of the facial muscles on the same side.
- Trousseau sign involves inflating a blood pressure cuff above the systolic pressure for 3 minutes, resulting in muscular contraction with flexion of the wrist, thumbs, and metacarpophalangeal joints and hyperextension of the fingers.
- Although symptoms of hypocalcemia are predominantly neuromuscular and include weakness, tetany, confusion and seizures, hypocalcemia can also cause arrhythmias, decrease in myocardial contractility, heart failure, and hypotension.
- Hypocalcemia usually develops in association with other electrolyte abnormalities such as hyperkalemia and hypomagnesemia. The combination of hypocalcemia and hyperkalemia is commonly seen in patients with renal failure.
Treatment of Hypocalcemia
- Treatment of hypocalcemia includes measurement of the ionized level of serum. When symptoms are present, calcium should be given intravenously even before the result of ionized calcium is available.
- Between 100 and 300 mg of elemental calcium is given intravenously, which will increase serum calcium for 1 to 2 hours; thus, repeated doses may be necessary.
- Calcium is given as calcium chloride or calcium gluconate. Calcium chloride has a higher amount of elemental calcium compared to calcium gluconate:
- Calcium chloride 10% 10 mL contains 360 mg of elemental calcium, whereas calcium gluconate 10% 10 mL contains 93 mg of elemental calcium.
- Calcium is given IV over 10 minutes (90 to 180 mg elemental calcium) followed by an IV drip of 540 to 720 mg in 500 to 1,000 mL D5W. The serum calcium level should be monitored every 4 to 6 hours and maintained at the low normal range of 7 to 9 mg/dL.
- Calcium should be injected cautiously to patients receiving digitalis because it may cause digitalis toxicity.
- If symptoms are not present, oral calcium supplements 1 to 4 g daily in divided doses may suffice.
- Therapy includes correction of other electrolyte abnormalities because calcium entry into the cells is dependent on the presence of normal levels of magnesium and potassium.
Prognosis
Prognosis of patients with hypocalcemia will depend on the underlying medical condition.
Topics Related to Hypokalemia:
- Hyperkalemia
- Basic Principles
- The Electrical Axis
- Left Ventricular Hypertrophy
- Right Bundle Branch block
- Left bundle Branch Block